Rwanda: Managing newborns with respiratory problems in Barame supported hospitals
During the delivery the first sign of live birth is a cry, the baby cries because air enters her lungs which then start to work. A healthy baby will continue to breath normally by her own without any other support. Although there might be other things to be observed during the first 10 minutes of life, breathing is key. Some babies during their early life and likely if they are premature, may have difficulty in breathing (respiratory distress or birth asphyxia) requiring support for breathing to avoid early death or irreversible brain damage due to deprivation of oxygen. For those cases, urgent appropriate measures should be taken by skilled health workers with appropriate equipment.
To reduce the neonatal death and the complications related to the respiratory problems that can occur early after birth, Enabel’s Barame project has developed and implemented two strategies at hospital level: (i)staff skills improvement via training and mentorship, and (ii) procurement of equipment.
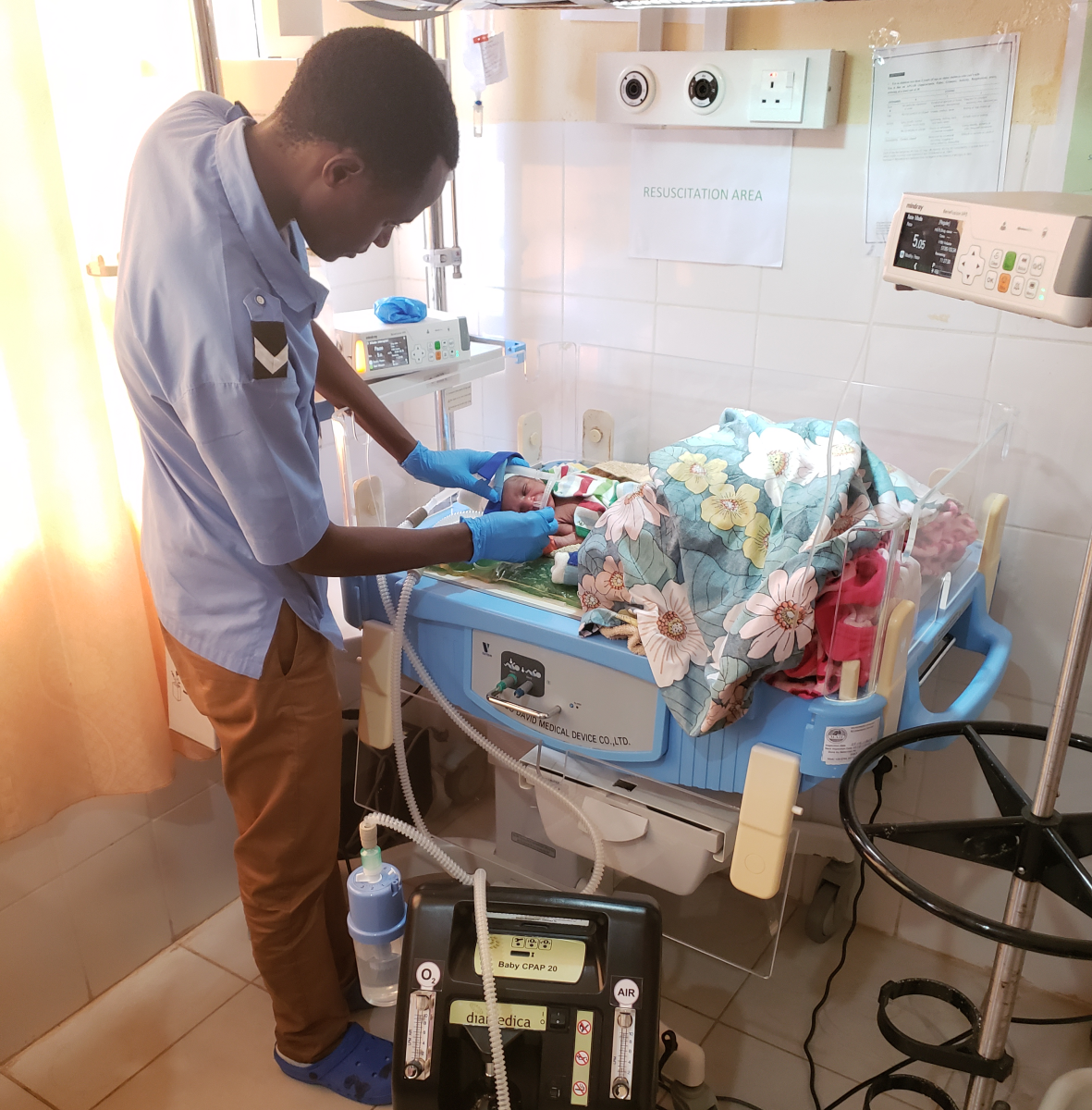
Last year (2022), the project procured an essential device, Continuous Positive Air Pressure (CPAP) to reduce the mortality and the complications related to respiratory distress at birth in seven hospitals which did not have it (2 in Rusizi, 2 in Nyamasheke and 3 in Karongi). The CPAP is a breathing therapy device that delivers air to a mask worn over the nose and/or mouth to help consistent breathing for neonates with either upper airway obstruction or respiratory failure; and the health care providers can easily adjust the quantity of needed oxygen. Numerous other equipment was also provided to support treatment and cares for neonates including oxygen cylinders and oxygen concentrators, infant incubator and complete resuscitation kits.
care providers from 14 hospitals were trained on management of baby born with respiratory difficulties and distress that include the adequate use of CPAP device, the newborn resuscitations measures and the good and safe use of oxygen. Mentees are now comfortable in using the respiratory machine on newborn babies and to conduct resuscitation on standard way.
Mme Manishimwe Annuarite, a nurse from Kinihira hospital, who followed the mentorship said “the use of this breathing machine has helped to reduce the level of not needed quantity oxygen by calibrating and monitoring the right quantity needed by the sick babies. There is a huge difference in using the electrical air-oxygen blending machine compared to mechanical (handmade) equipment we had before. The unnecessary oxygen was considerably reduced, allowing the use of blended air-oxygen at the satisfactory level compatible with the capacity of infants”.
Mentors and mentees confirmed that the use of the received machines has shortened the time newborn with breathing difficulties passes on respiratory support and has contributed to reduce the mortality.
Latest news from this project
No news